Why Do Leg Veins Bulge? The Real Cause of Varicose Veins
Have you ever noticed blue, bulging veins on someone’s legs — or even your own?
This condition is called varicose veins.
It affects about one in three adults, and is especially common among women.
While many think it’s just a cosmetic issue, leaving it untreated can lead to leg heaviness, swelling, inflammation, or even skin ulcers.

Saphenous-type varicose veins in the thigh
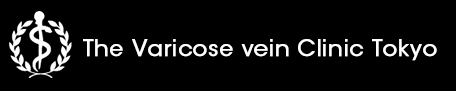
So, why do veins become swollen and bumpy?
Based on the latest medical research, this article explains “how varicose veins form” in a way that even high school students can understand.
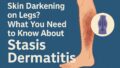
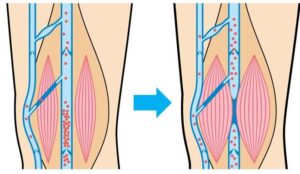
1. When Blood Starts to Flow Backward
In our bodies, blood is pumped from the heart throughout the body and then returns through the veins.
To move blood from the lower body back up to the heart, veins must work against gravity.
Here, small structures called venous valves act like “gates,” allowing blood to flow upward but closing tightly to prevent it from falling back down.
However, standing for long hours, aging, or lack of exercise can damage these valves.
When that happens, blood begins to flow backward, creating a “traffic jam” in the veins.
As pressure builds up, the veins expand and bulge under the skin — forming the characteristic varicose veins.
How varicose veins develop
In other words, varicose veins are like a “broken one-way ticket” for your blood.
2. Like an Old Rubber Hose
Healthy veins are flexible and elastic, but as we age, they become stiff — just like an old rubber hose.
Inside the body, the balance of two key proteins — collagen and elastin — begins to shift, causing the vein walls to stretch and lose their ability to contract.
Research has shown that patients with varicose veins have an abnormal ratio of collagen type I to type III, making their vein walls rigid and fragile.
In short, the veins lose elasticity and can no longer withstand blood pressure, leading them to bulge and twist.
3. Inflammation “Rusts” the Veins
When blood flow stagnates, inflammation occurs inside the veins.
Inflammation is the body’s natural repair response, but if it continues too long, it starts to damage the tissue itself.
During inflammation, white blood cells and platelets release reactive oxygen species (ROS) — the molecular equivalent of “rust.”
These oxidants attack the inner lining of the vein (the endothelium), gradually eroding and weakening it.
It’s similar to how rust slowly eats away at an iron pipe.
If left untreated, this damage worsens, trapping the veins in a vicious cycle of inflammation and stagnation.
4. Oxygen Deprivation Weakens the Veins
When blood moves slowly, vein cells become deprived of oxygen.
In response, they send signals to widen the veins and produce an enzyme called MMP (matrix metalloproteinase) — a kind of “molecular scissors.”
While MMP normally helps rebuild tissue, excessive activity can degrade the vein wall itself, making it thinner and more fragile.
5. The “Rust Reaction” of Red Blood Cells
Another key factor involves changes in red blood cells.
These cells usually act as oxygen couriers, but when congestion persists, they break apart, releasing hemoglobin into the surrounding tissue.
Hemoglobin reacts with oxygen and hydrogen peroxide — just like iron rusting when exposed to moisture — producing oxidative stress that damages nearby blood vessels even more.
It’s literally a “rusting” process within your veins.
6. Lifestyle and Genetic Factors
Varicose veins often result from a combination of genetics and lifestyle.
If your parents have varicose veins, your risk is higher.
Jobs that involve prolonged standing (like hairdressers, chefs, or sales staff) or sitting (desk work, drivers), as well as obesity, inactivity, smoking, and female hormones (pregnancy, childbirth, menopause), all increase the risk.
In short, when “standing too long + not moving + aging + heredity” come together, your veins start sending out an SOS signal.
7. How Can You Prevent It?
To prevent varicose veins, it’s essential to keep your blood flowing smoothly.
Here are three practical tips:
① Move Your Legs
Your calf muscles are known as the “second heart.”
Walking or standing on your tiptoes helps those muscles pump blood upward.
second heart
② Elevate Your Legs
When resting or sleeping, raise your legs slightly to let gravity assist blood flow back to the heart.
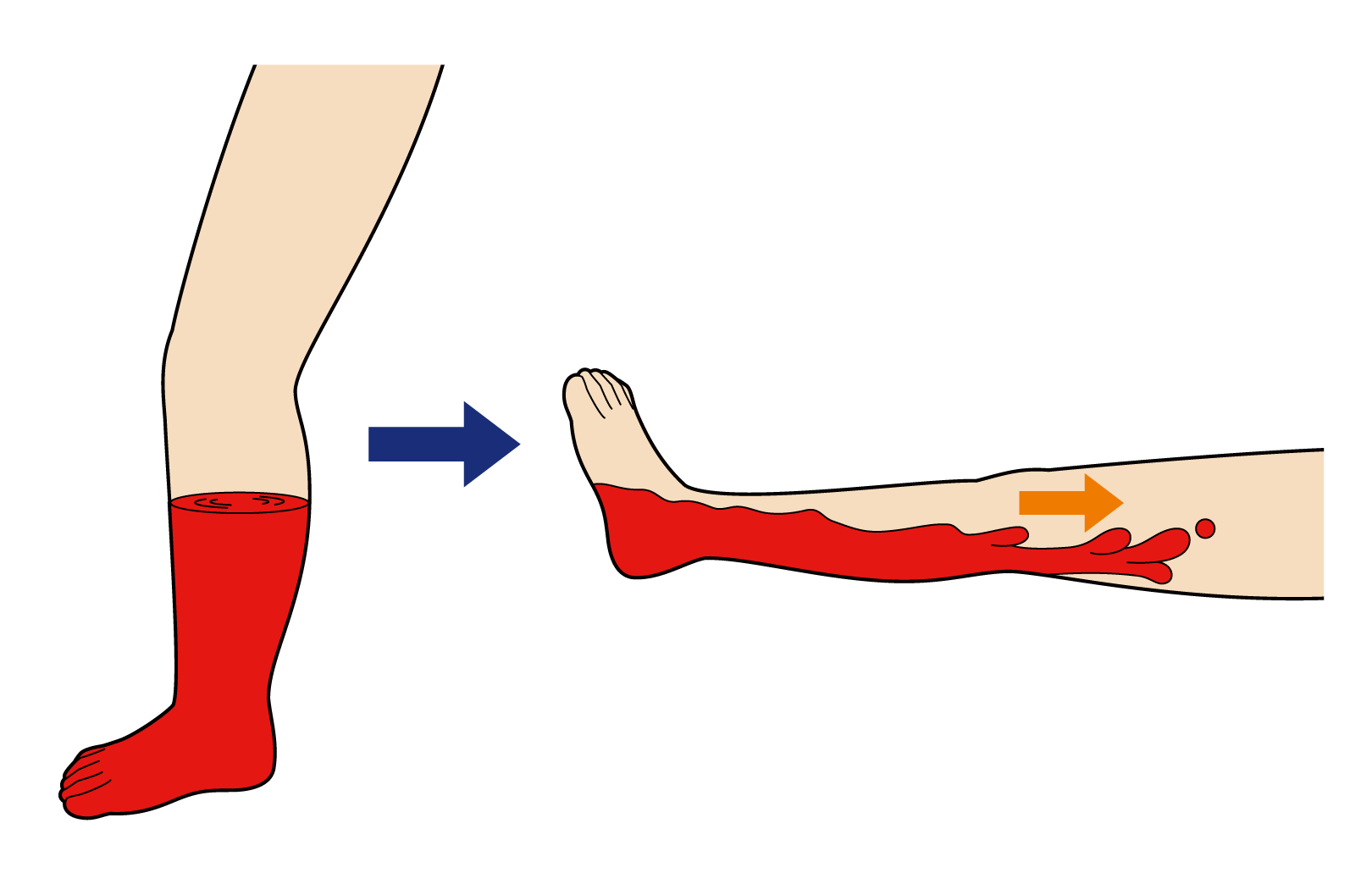
Raising your legs helps blood return naturally
③ Wear Compression Stockings
Gentle pressure on the legs prevents blood from pooling and improves circulation.
Nowadays, many compression stockings come in stylish designs, making them easier for young people to wear daily.

Knee-high compression stockings
8. Nutrients That Protect Your Veins
Studies have found that some natural compounds can help protect blood vessels.
For example, diosmin and hesperidin (found in citrus peels) and pycnogenol (from pine bark or chestnut skin) have antioxidant and anti-inflammatory effects.
These act like “anti-rust coatings” for your veins, improving blood flow and reducing oxidative damage.
9. In Summary: Varicose Veins Are an SOS From Your Veins
Varicose veins are not just a cosmetic issue.
They’re a sign of “vascular aging,” where poor blood flow, inflammation, and oxidative stress gradually weaken the veins.
The good news is that it’s a preventable condition.
Simple habits — moving your legs, avoiding prolonged postures, resting your feet — can greatly reduce vein stress.
Once damaged, veins are difficult to restore.
That’s why early care is the best treatment.
Reference:
Gwozdzinski L, Pieniazek A, Gwozdzinski K. Factors Influencing Venous Remodeling in the Development of Varicose Veins of the Lower Limbs.
International Journal of Molecular Sciences. 2024;25:1560.