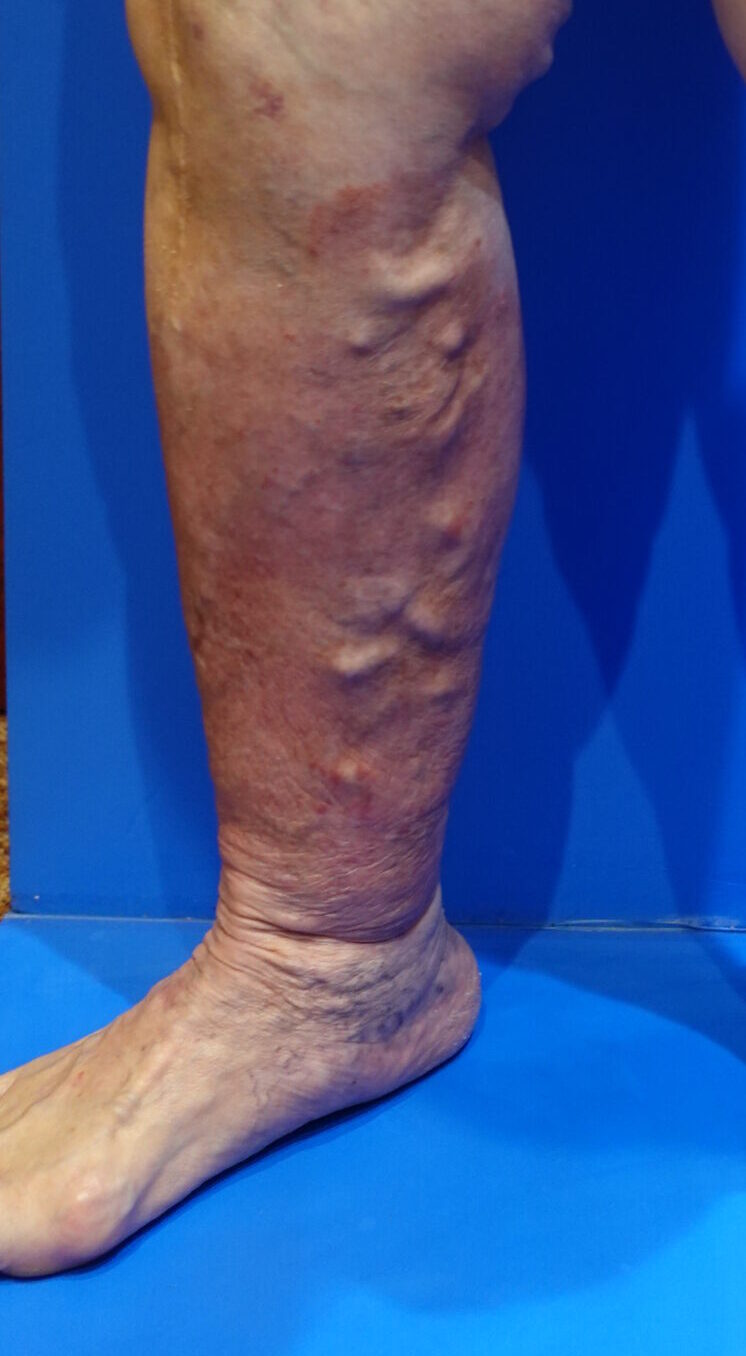
Understanding Skin Hardening Symptoms and Their Relation to Varicose Veins
Varicose veins refer to a condition in which the veins in the legs become enlarged and twisted. This condition not only affects the appearance of the legs but can also lead to serious skin problems if left untreated. One of these complications is the hardening of the skin. In this blog, we will explore the connection between skin hardening and varicose veins and introduce preventive measures.
What Causes Skin Hardening?
Skin hardening is one of the common complications that occurs as varicose veins progress. When blood circulation in the legs worsens, blood begins to pool in the veins, and the tissues no longer receive adequate oxygen and nutrients. Over time, this leads to a condition called ” lipodermatosclerosis “, where the skin becomes hard.
Lipodermatosclerosis is characterized by the skin turning brown or reddish-brown and becoming thick and stiff. This hardening occurs due to inflammation and fibrosis of the subcutaneous fat tissue. As a result, the skin not only becomes hard but may also cause pain and itching.

The Connection Between Varicose Veins and Skin Hardening
When blood pools due to varicose veins, it places stress on the skin, accelerating the hardening process. The following mechanisms are involved:
Blood Reflux: When the valves in the leg veins don’t function properly, blood tends to flow backward due to gravity, accumulating in the lower leg. This increases pressure in the veins and affects the surrounding tissue.
Chronic Inflammation: Stagnant blood can lead to chronic inflammation in the skin and subcutaneous tissues. Repeated inflammation causes tissue hardening, resulting in lipodermatosclerosis.
Oxygen Deprivation: When blood pools due to varicose veins, oxygen supply to the skin decreases, lowering tissue metabolism and accelerating skin hardening.
Prevention and Treatment
Early intervention is key to preventing skin hardening. The following measures can help slow the progression of varicose veins and maintain skin health:
Early Treatment: If varicose veins are suspected, it’s essential to seek consultation with a specialist and undergo appropriate treatment. Treatment options include compression therapy, laser therapy, and glue treatment, depending on the condition.
Regular Exercise: Moderate exercise promotes blood circulation and helps maintain vein health. Walking and stretching are particularly recommended.
Compression Therapy: Using compression stockings (elastic stockings) under medical supervision can prevent blood pooling and slow the progression of varicose veins.
Skin Care: Regular use of moisturizing creams or lotions to care for the skin is important before hardening occurs. If hardening is noticed, consult a specialist early.
The Risk of Lipodermatosclerosis and Skin Ulcers
Lipodermatosclerosis is not only characterized by skin hardening but also increases the risk of developing severe skin ulcers. As varicose veins progress, stagnant blood and chronic inflammation can cause the skin to thin, making ulcers more likely to form. These ulcers heal slowly and have a high risk of infection, requiring prompt attention.
Why You Should Consult a Vascular Surgeon
Varicose veins and skin hardening are closely related, making early treatment crucial. If you experience symptoms of varicose veins or lipodermatosclerosis, it’s highly recommended that you consult a vascular surgeon. A specialist can provide accurate diagnosis and treatment, helping prevent the formation of skin ulcers. Early intervention can improve skin condition and avoid serious complications.